A Common Set of Recommendations for Various Musculoskeletal Conditions
A recent paper published in the British Journal of Sports Medicine reviewed a number of clinical practise guidelines and provided a list of best practises in musculoskeletal medicine. Before delving into the clinical gems of this paper, it’s important to remind our readers of the high quality of this information. To be blunt, this is not just someone sharing their opinion. These are a list of recommendations derived from a huge body of high-quality scientific evidence.
Clinical Practise Guidelines
A systematic review compiles a large number of published research papers, pools the findings, and gives the reader a summarized impression of what the science supports. Clinical practise guidelines are the work of a panel of experts who gather the literature (similar to a systematic review) and then make recommendations for practitioners on a good way to streamline evidence-based practise. The paper mentioned at the beginning of this blog (and the focus of this blog entry) was published in 2020, and it aimed to identify a common set of recommendations from high-quality clinical practise guidelines for various musculoskeletal conditions. In total, they reviewed and summarized the pertinent and consistent recommendations from 44 clinical practise guidelines. In a sense, this paper is a systematic review of systematic reviews so it can be considered a fairly high level of evidence.
The consistent recommendations were as follows:
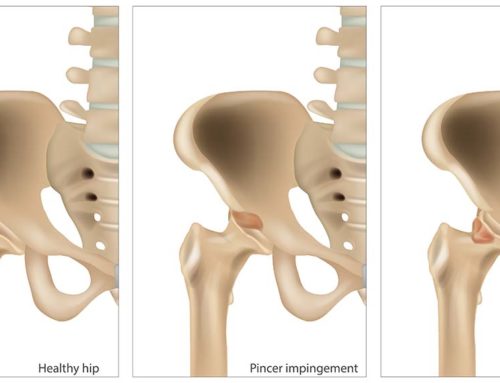
- X-rays and imaging are perhaps overused. It should only be ordered if there is concern of something serious (such as cancer or infection), if someone’s condition hasn’t improved despite good treatment or if the imaging is likely to change how the condition is managed.
- Conservative treatment for musculoskeletal conditions should be attempted prior to any surgery (apart from extenuating circumstances like fracture or cancer). For example, unless there is a full thickness rotator cuff tear discovered, surgery for rotator cuff injury should not be considered until three months of non-surgical management was unsuccessful.
- All conservative management (such as chiropractic, physiotherapy and massage therapy) should be individualized and focused on the patient. Patients should be appropriately educated about their condition and their recovery strategy, and they should share in the decision-making process.
- Self-management of any injury is encouraged. Re-examinations should occur regularly to ensure that a patient is progressing appropriately.
- Practitioners should know how to screen patients and identify those with a serious pathology.
- Exercise should be a part of every treatment program. Manual therapy should only be used in conjunction with another type of intervention. These other interventions can include exercise, counselling, education or activity advice. Manual therapy should not be used as a standalone treatment without adding in any of the above.
- Continuing or returning to work is something that should be encouraged and should occur as soon as realistically possible.
- For osteoarthritis specifically, self-management is valuable. Those individuals who are overweight/obese should attempt to reduce their weight to reduce the compressive load on the joint. Glucosamine or chondroitin is not recommended for structural change related to osteoarthritis.
- For knees, in particular, arthroscopic debridement surgeries are not recommended unless there is an obvious locking in the joint from a loose body. In simple terms, arthroscopic surgeries described as “clean ups” aren’t recommended unless there is a specific structure that is being targeted.
- Spinal injections (e.g., facet joint injections, medial branch blocks, intradiscal injections, prolotherapy, and trigger point injections) should not be used for lower back pain.
Evidence Informed Treatment
Evidence informed treatment is a model of care that combines an understanding of the best evidence with practitioner experience and patient input. The aforementioned points are supported by the bulk of the existing literature, but they don’t pertain to every situation. Good evidence informed care takes points like these and filter them with experience and what is suitable for that patient’s individuality. Everyone is different and so is their injury. At the same time, these points should help serve as a general compass for decision making in appropriate circumstances.
Are you injured or in pain? Give us a call, we can help!
By Dr. Kevin McIntyre B.Kin., DC
References
Lin I, Wiles L, Waller R, et al. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. British Journal of Sports Medicine 2020; 59: 79-86.